Unwinding Medicaid Continuous Coverage: Understanding the Importance of a Solid Eligibility Verification Strategy and PBE
SSI Healthcare Rev Cycle Solutions
JANUARY 17, 2023
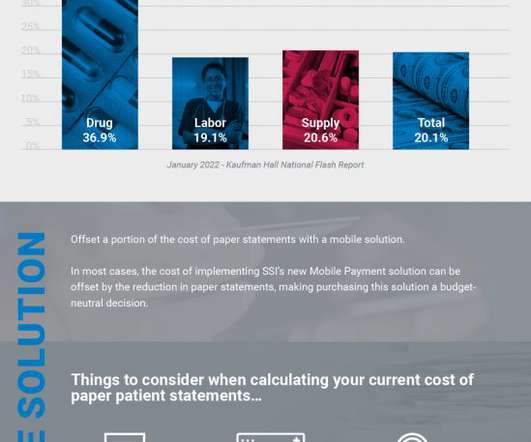
This could result in an increased burden on hospitals to screen patients for charity care, financial assistance, and collection activity. For more information on SSI PBE, contact us or request a demo. Click the button below to receive a customized tutorial catered to your specific revenue cycle management (RCM) needs.















Let's personalize your content